Ultraprocessed foods can promote the onset and worsening of inflammatory bowel disease. The hypothesis, supported by extensive scientific literature, is retraced by a Belgian study through analysis of the function played by each non-nutritive substance typical of ultra-processed foods in the manifestation of intestinal inflammation. (1)
Ultraprocessed foods and inflammatory bowel disease
Ultraprocessed foods are ready-to-eat industrial products characterized by
– High amounts of sugar, saturated fat and salt,
– Low amounts of protein, fiber, vitamins and minerals,
– Presence of various preservative additives, stabilizers and thickeners, emulsifiers, artificial sweeteners and colorants,
– Unrepeatable industrial processing in domestic kitchens: hydrogenation, hydrolyzing, extrusion, fractionation, etc. Processes that aim to make highly palatable, ready-to-eat, highly profitable, long shelf life foods.
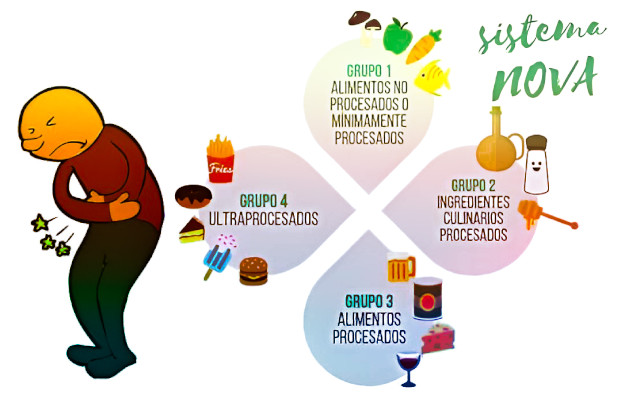
Generally, these are snacks, pastries, soft drinks, ready meals, and processed meats. Products that fall under group 4 of the Nova classification. To recognize them at a glance, just use nutrition label decoding systems, such as the Yuka app, based on NutriScore.
Regular consumption of ultra-processed foods is correlated with increased risk of chronicNon-Communicable Diseases (NCDs), such as obesity, diabetes, cardiovascular disease, cancer and, indeed, inflammatory bowel disease, including Crohn’s disease and ulcerative colitis. (2)
The role of diet
These gut diseases appear to occur in genetically predisposed individuals upon the occurrence of some interaction between the microbiota, immune system, and environmental factors such as smoking, antibiotic use, and diet.
In particular, the Western diet -that is, the ‘Western diet’ high in fat, sugar and salt(HFSS) and full of additives-is considered a crucial factor in the onset and worsening of inflammatory bowel disease.
Not surprisingly, the incidence of these diseases increases as consumption of ultra-processed foods spreads to newly industrialized regions, Africa and South America, and stabilizes (in some declines) in Western countries such as Europe and North America, the researchers point out.
Ingredients that are enemies of the intestinal barrier
This study reviews substances recognized in the scientific literature as capable of affecting the intestinal barrier and increasing intestinal permeability and promoting inflammation. A harmful action that can manifest itself by altering the components of the barrier (mucosal layer, epithelial cells, immune cells) or altering the composition of the microbiota.
Emulsifiers and thickeners
Emulsifiers such as carrageenan, carboxymethylcellulose, polysorbate-80, and mono- and diglycerides of fatty acids are very common in ultra-processed foods. And mind you, not only in chocolates or snacks, but even in the milk snacks so beloved by children, ice cream, fresh pasta, and spreadable cheeses, as we have reported several times. (3)
These additives have been identified through in vitro and animal studies as harmful to each component of the intestinal barrier and therefore promoters of inflammatory bowel disease.
Human clinical studies confirm the evidence. The researchers cite four in which emulsifier consumption caused altered microbiota, thinning of intestinal mucus, worsening of intestinal inflammation, and increased recurrence.
Azo dyes
Azo dyes are still widely used in foods, particularly in candies, dairy products and beverages. They are known to promote neurobehavioral abnormalities in children, such as hyperactivity.
Two of these synthetic dyes, Red 40 and Yellow 6, are considered safe for human consumption, according to the WHO. However, a recent study (He et al.) in guinea pigs showed that the two azo dyes can trigger or aggravate inflammatory bowel disease.
In our market surveys we found Red 40 (E 129, Allura Red or Allura Red) in the Breezer Ruby Grapefruit and Bacardi Breezer Peach alcoholpops. Orange Yellow (Yellow 6o Sunset Yellow, Sunset Yellow, E110), on the other hand, we identified it in Ginger San Benedetto and Aperol.
Titanium dioxide
Titanium dioxide (TiO 2, E171) is used as a food additive for its bleaching and brightening properties. It is mainly added in confectionery, candies and chewing gum, white sauces and glazes, and also in toothpastes and pharmaceuticals.
It is one-third composed of nanoparticles (<100 nm) that accumulate in vital organs, liver and spleen especially. It is neurotoxic, causes inflammation, and induces changes in the intestines (colon and rectum) that can develop into tumors over time. And it is genotoxic, that is, capable of damaging DNA.
In Europe since 7.2.22 it has been prohibited to add it in foods and food supplements, but it remains in medicines and toothpastes, as we have seen.
Artificial sweeteners
In vitro and animal studies have shown that artificial sweeteners, such as sucralose, aspartame, and saccharin, can interact with several components of the intestinal barrier and promote intestinal inflammation.
Human studies, however, are scarce and contradictory. Therefore, synthetic sweeteners remain widely present in foods labeled as ‘no added sugar.’
Halls
Ultraprocessed foods generally contain a very high salt content. Food salt or sodium chloride (NaCl) is composed of 40 percent sodium and 60 percent chloride.
WHO recommends consuming no more than 5 g of salt per day, but this threshold is often exceeded. This is despite the fact that the link between excessive salt intake and hypertension, other cardiovascular diseases, and an increased risk of premature death is now well known.
The study authors report that both in vitro and in vivo studies suggest that excessive salt intake may also modulate the immune system, and in this way be involved in the development of inflammatory bowel disease.
Phosphate
Inorganic phosphate is often present in ultra-processed foods through various food additives, added with an emulsifying (e.g., sodium phosphate, E 339) or antioxidant (e.g., phosphoric acid, E338) function.
These additives are permitted in a hundred foods, and recent studies have found a generalized increase in the level of phosphate in the population’s blood vessel wall, a condition that increases cardiovascular risk.
The only study, with in vitro and in vivo experiments, identified by the researchers shows that excessive dietary phosphate intake can exacerbate intestinal inflammation. (4)
Conclusions
‘Preclinical studies show that several nonnutritive components of UPFs (ultra-processed foods, ed.) can adversely affect the intestinal barrier. They can induce dysbiosis, negatively affect the mucus layer, increase the permeability of the intestinal epithelium, or interact directly with the immune system.
Based on these findings, a diet low in UPFs (ultra-processed foods, ed) could potentially induce remission or control symptoms in patients with IBD (inflammatory bowel disease, ed).
However, human data are still limited, and nutritional studies are needed to evaluate the clinical potential of new dietary therapies for IBD patients. Meanwhile, it is reasonable to advise our patients with IBD to reduce the intake of UPF‘, the researchers conclude.
Notes
(1) Vissers Eva, Wellens Judith, Sabino João. Ultra-processed foods as a possible culprit for the rising prevalence of inflammatory bowel diseases. Frontiers in Medicine, vol. 9, 2022. https://www.frontiersin.org/articles/10.3389/fmed.2022.1058373
(2) The correlation between regular consumption of ultra-processed foods and noncommunicable diseases is so pronounced that it has prompted a group of nutrition scientists to appeal to the UN to urge governments to adopt nutritional policies to curb such consumption. V. Dario Dongo, Andrea Adelmo Della Penna. Ultraprocessed foods, the worst evil. Appeal of scientists in the British Medical Journal. GIFT (Great Italian Food Trade). 16.8.21
(3) See previous articles by Marta Strinati on GIFT (Great Italian Food Trade):
- Tzatziki sauce, beware of ingredients. 21.7.22
- Risk additives in Daygum Ferragni gum. 17.7.22
- Fresh stuffed pasta, the taste of misleading labels. 38 products compared. 10.2.22
- Corn flakes and filled cereals, 24 compared. 22.1.22.
- Frùttolo and other milk snacks, 10 products compared. 25.9.21
- Fresh cheese spreads and flakes, 18 products compared. 30.7.21
- Packaged ice cream, too many suspicious additives. Our market survey of 20 products. 6.7.21
(4) Sugihara K, Masuda M, Nakao M, Abuduli M, Imi Y, Oda N, et al. Dietary phosphate exacerbates intestinal inflammation in experimental colitis. J Clin Biochem Nutr. (2017) 61:91-9. doi: 10.3164/jcbn.16-117
Professional journalist since January 1995, he has worked for newspapers (Il Messaggero, Paese Sera, La Stampa) and periodicals (NumeroUno, Il Salvagente). She is the author of journalistic surveys on food, she has published the book "Reading labels to know what we eat".